Preeclampsia Linked to Increased Markers of Brain Inflammation and Alzheimer Disease
A study presented at the Alzheimer Association International Congress 2022 (AAIC2022), showed an association between history of severe preeclampsia and high levels of extracellular vesicles (EVs)--vascular particles--carrying markers of inflammation and Alzheimer disease (AD).
Those who had experienced severe preeclampsia vs mild or no preeclampsia had significantly higher levels of EVs positive for low-density lipoprotein receptor (LDL-R), a marker of blood-brain barrier endothelial damage, and tissue factor, an inflammatory coagulation pathway activator. Plasma concentration of total amyloid-β was also significantly greater in people with history of severe vs mild preeclampsia.
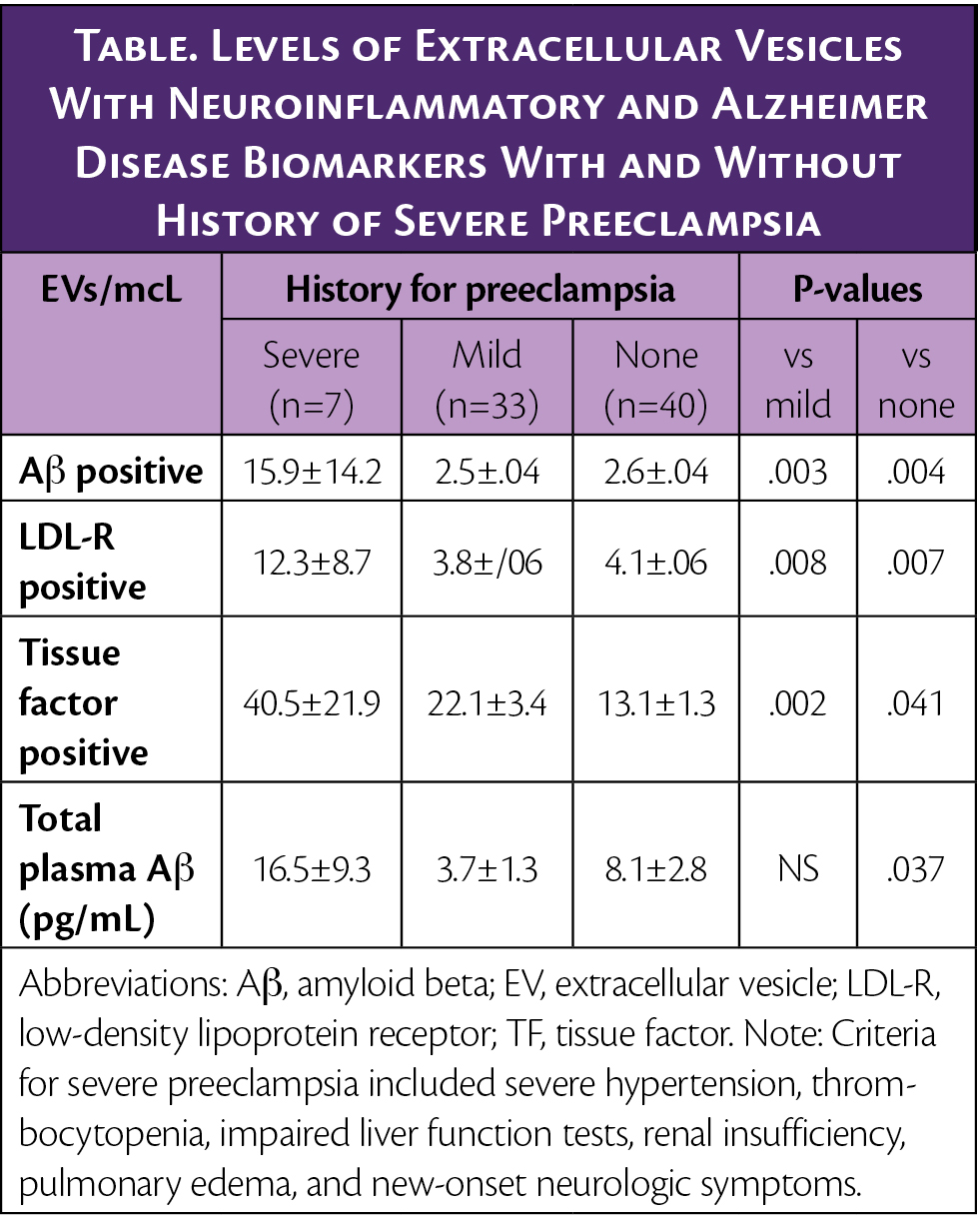
The number of tissue factor positive EVs was negatively correlated with total gray matter volume (cm3) (P<.05).
“These findings indicate that people with a history of preeclampsia have increased levels of markers of neurovascular damage which may negatively impact their cognitive skills,” said Sonja Suvakov, MD, PhD, assistant professor of medicine, Mayo Clinic. “Further research is required to fully understand the neurodegenerative and cognitive risks that a history of hypertensive disorders confers on people throughout life.”
Data for this study came from the Rochester Epidemiology Project.Blood-borne EVs derived from neurovascular cellular activation were determined by standardized digital flow cytometry. Plasma concentration of amyloid-β was measured by ELISA. Differences among the groups were tested by ANOVA, with the least difference test for post hoc analysis. The association between EVs and MRI brain imaging was assessed by Pearson correlation coefficient.
