Outcomes After Acute Ischemic Stroke Noninferior With CT Alone Vs CT Plus Follow-Up MRI
As published in JAMA Network Open, a study by Heitor Cabral Frade and colleagues at the University of Texas Medical Branch at Galveston and the University of North Carolina School of Medicine, Chapel Hill showed outcomes of acute ischemic stroke were noninferior with initial CT vs initial CT plus MRI. Outcomes for both groups in a propensity score-matched cohort are shown in the Table.
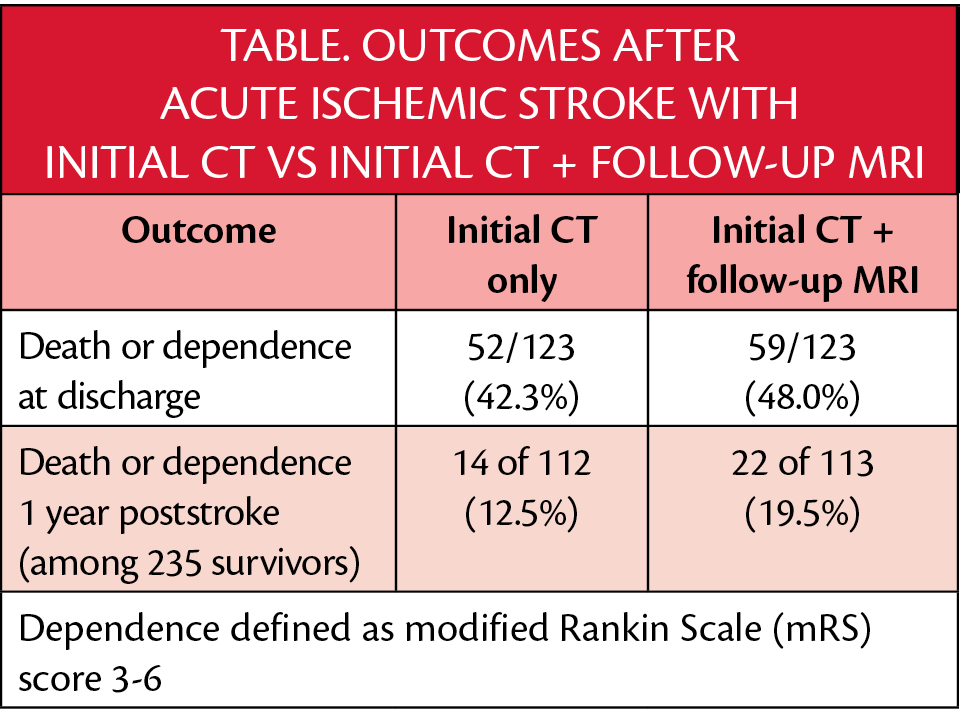
With CT+MRI compared with CT alone, 5.7% (95% CI: -6.7% to 18.1%) more participants died in the hospital or were dependent at discharge. For the 235 survivors, those who had both imaging studies had a relative risk of death/dependence of 1.14 (95% CI: 0.86-1.5). Based on the designs of prior randomized clinical trials for treatment of ischemic stroke treatments, these differences met the -7.5% noninferiority criteria of -7.5% for absolute differences and 0.725 for relative risk. The authors concluded that further research is needed to determine which patients hospitalized with acute ischemic stroke on initial CT benefit from follow-up MRI.
An invited commentary from Bruce Campbell of the University of Melbourne, Parkville, Victoria, Australia posited that a diagnostic test could not affect outcomes and that other factors that led to a follow-up MRI may have artifactually led to statistically equivalent outcomes between the 2 groups. Campbell also suggested the cost of obtaining further proof for the benefit of follow-up MRI could outweigh the cost in time, effect on study participants, and resources for obtaining such evidence.
In contrast, in a second invited commentary, Michael Teitcher and José Biller of Loyola University Chicago Stritch School of Medicine, made the point that the propensity score-balanced comparison sufficiently controlled for differences and supported the evidence of noninferiority. Teitcher and Biller suggested that clinicians should consider whether the information to be gained with follow-up MRI will meaningfully affect patient outcomes rather than routinely ordering follow-up MRI for all recovering from stroke.
Data for the study by Cabral Frade et al. came from electronic medical records of individuals who were admitted to the hospital with an acute ischemic stroke diagnosed by CT between 2015 and 2017. Of 508 cases, 123 individuals had poststroke follow-up MRI; these cases were propensity matched to cases with initial CT only. Individuals in this study (n=246) were median age 68 (interquartile range [IQR] 58-78.8); sex of participants was reported as male (n=131) or female (n=125) and gender was not reported.
