Neurologic Recovery After Severe COVID-19 Leaves One-Third With Worsening Cognitive Symptoms at 12 Months
Among individuals who were admitted to the intensive care unit with COVID-19, outcomes were worse for those who had neurologic symptoms both in hospital and over 12 months after COVID-19 diagnosis, including cognitive deficits in 41%, regardless of whether they had neurologic symptoms while in the ICU. For a sizable minority, objective symptoms continued to worsen between 6 and 12 months after COVID-19 diagnosis.
Of 4,491 patients in ICU with COVID-19, 606 (13.5%) had new neurologic events, that occurred a median 2 days after COVID-19 symptoms. Intubation was required for 22% of all patients and 40% of those with neurology symptoms. Toxic or metabolic encephalopathy was most common (57%), followed by seizure (12%), ischemic stroke or anoxia/hypoxia (10% each), movement disorder (7%), and hemorrhagic stroke (4%).
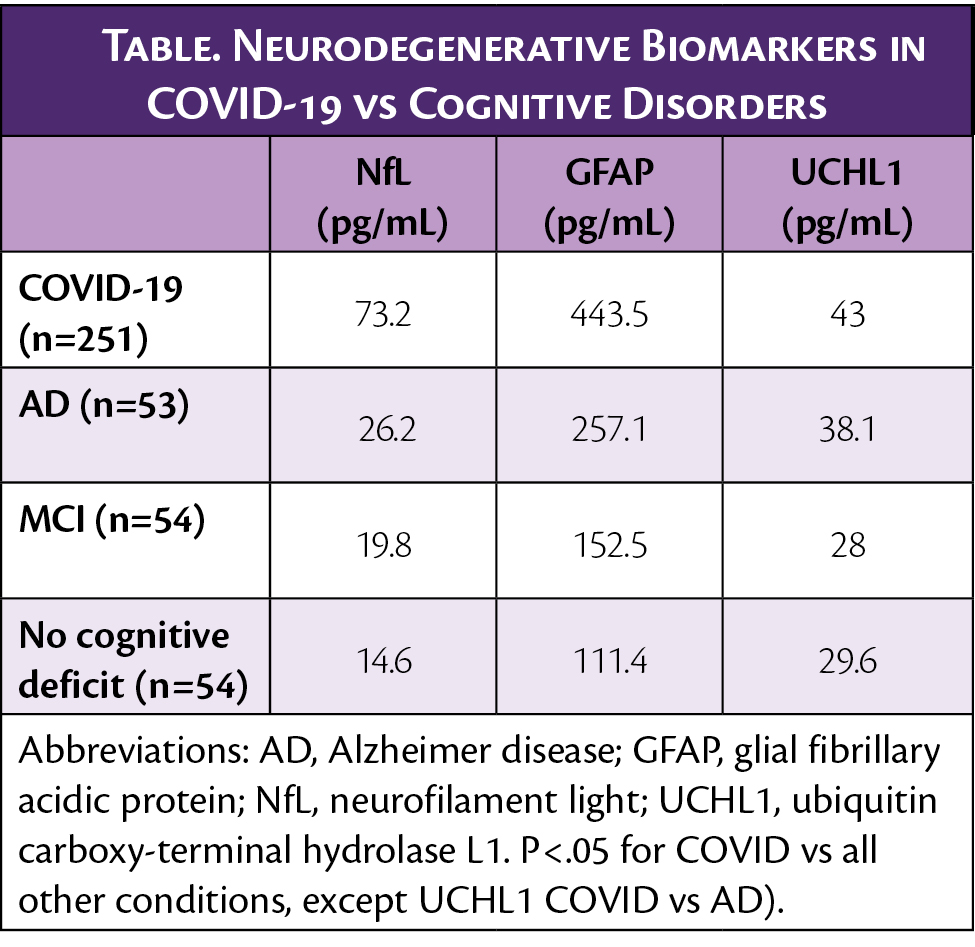
In a cohort of 251 individuals in the ICU with COVID-19 and neurologic symptoms, biomarkers of degeneration were elevated at admission to the hospital (Table), not only above normal, but for neurofilament light (NfL) and glial fibrillary acidic protein (GFAP), above the levels seen in people with Alzheimer disease (AD).
Among those with (n=113) or without (n=129) neurologic symptoms who had follow-up at 12 months, 50% reported still having symptoms, most commonly headache, shortness of breath, or brain fog, and 71% of these individuals had more than 1 symptom of long COVID as defined by the Centers for Disease Control (CDC).
With cluster analysis, 3 groups of patients were identified: 1) those with a median 1 symptom (37%); 2) those with a few symptoms (50%); and 3) those with many symptoms. The number of symptoms correlated with the number of therapies used to treat long COVID, and 83% had at least some improvement with those therapies.
Objective measures of the modified Rank scale (mRS), the Barthel index of activities of daily living, telephone-administered Montreal Cognitive Assessment (t-MoCA), and the neurologic quality of life (NeuroQoL) showed 87% of these individuals had at least 1 objectively measurable symptom. At 12 months, 41% had deficits on the t-MoCA, 36% had deficits on the Barthel index, and 34% had a poor mRS score (4-6). On the NeuroQoL at 12 months, 4% had depression, 9% fatigue, and 10% sleep difficulties. Notably, despite 41% having cognitive deficits on the t-MoCA, only 20% had reported brain fog or cognitive difficulties.
Among those who had follow up at both 6 and 12 months, improvements in the t-MoCA and anxiety improved as did sleep, fatigue, and depression. However, 25% to 33% not only did not improve, but had declines in these objective measures from months 6 to 12. Predictors of outcomes included severity of COVID-19, baseline disability, age, female sex, and life stressors (eg, socioecomoic status, death of a loved one, social isolation, and food insecurity). NfLlevels in a small number who had biomarker levels and 6- and 12-month follow up data suggests that NfL could also predict long COVID outcomes.
These data were presented at the Alzheimer Association International Congress 2022 (AAIC2022) in San Diego, CA and online.
