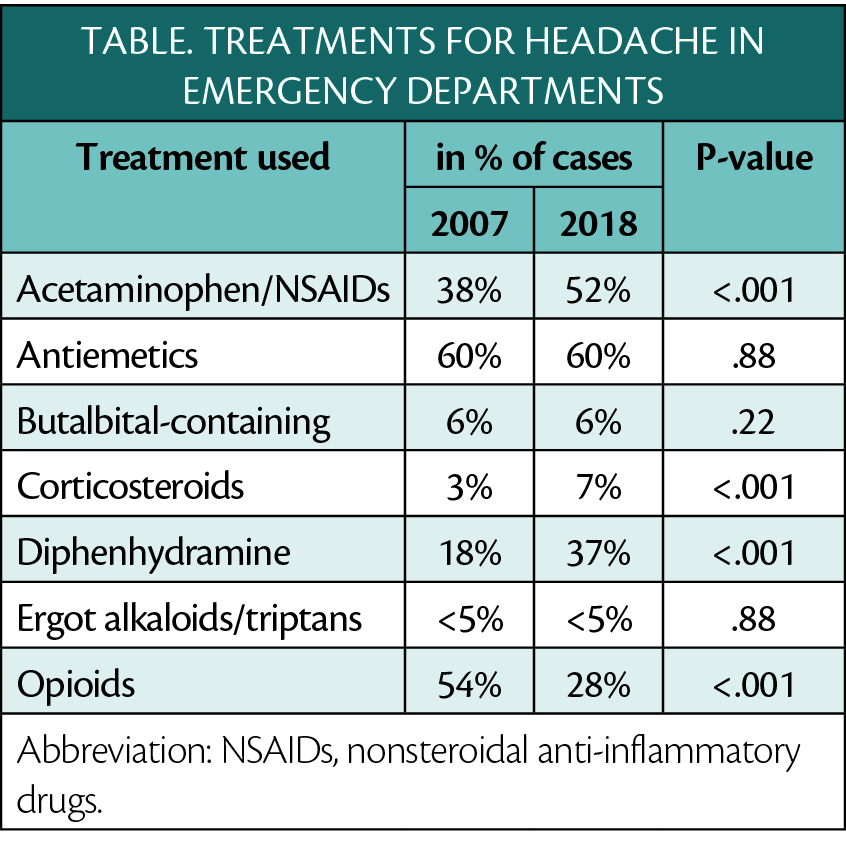
Headaches in Emergency Departments--Fewer Opioids and More Diphenhydramine, But Low Use of Migraine-Specific Treatments
American Headache Society clinical guidelines for parenteral treatment of severe headache in emergency settings recommend against use of both opioids and diphenhydramine. Use of opioids decreased from 2007 to 2018, but use of diphenhydramine remained high. Among recommended treatments, use of acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) increased and antiemetics remained high and stable. Use of recommended ergot alkaloids/triptans and corticosteroids remained low, although there was an increase in corticosteroid use.
In this study, out of 10.2 million visits for headache, 33.9% were migraine, 63.9 were not otherwise specified, and the remaining 3.2% were tension-type or trigeminal autonomic celphagia (TACs). Consultation from services outside the emergency department, including neurology, occurred in only 5% of these cases. Approximately one-third of visits including diagnostic neuroimaging.
These data come from a study presented at the American Headache Society Meeting June 9-12, Denver, CO that evaluated treatments given for all adults discharged with a headache diagnosis code in the 2007-2018 National Hospital Ambulatory Medical Care Survey (NHAMCS) database. The headaches diagnosed included migraine, tension-type headache, trigeminal autonomic cephalgia (TAC), and not otherwise specified. The NHAMCS data base is a nationally representative sample of ambulatory care centers in the US, reflecting real-world medication use.
