Consensus Definition of Refractory Migraine for Use in Veterans Health Developed by Workgroup
The Veterans Health Administration Headache Center of Excellence Refractory Workgroup presented their consensus definition of refractory migraine (RM) at the 65th Annual Meeting of the American Headache Society. To date, there has been a lack of a clear definition for RM in the field. The definition formalized by the Workgroup consists of 3 parts:
1. Pain that meets the International Classification of Headache Disorders, third edition (ICHD-3) criteria for migraine
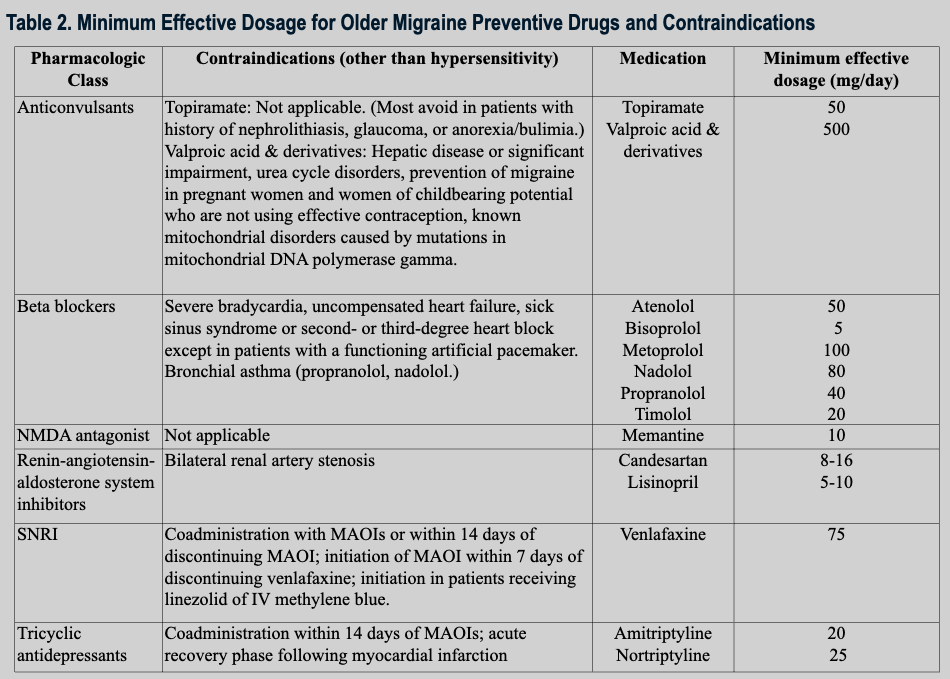
2. Failure of 3 of the following preventive medication classes: antidepressants, anticonvulsants, beta-blockers, calcitonin gene-related peptide monoclonal antibodies (CGRP mAbs), CGRP antagonists, renin-angiotensin-aldosterone system inhibitors, neurotoxins, and NMDA antagonists
3. An adequate trial period for the preventive medication consisting of 3 months at minimum effective or maximally tolerated dosage.
The Workgroup included Veterans Affairs (VA) clinicians with extensive experience in migraine management and direct patient care. Clinical pharmacist practitioners, psychiatrists, clinical health psychologists, and United Council for Neurologic Subspecialties (UCNS) Headache Medicine Certified neurologists were all represented in the group. The workgroup members conducted a systematic review of 3 refractory consensus statements as well as 6 research studies implementing those statements. The members were aligned with the statements regarding the medication classes included in the definition. However, they conducted a second, targeted review to determine the minimum effective dosage for each medication, because the initial review did not provide sufficient evidence.
The definition provided by the Workgroup is intended for implementation in the operationalization of RM in the Veterans Health Administration’s electronic health records. In the future, according to the group members Dr. Alexander B. Guirguis, PharmD, Dr. Vinh Dao, PharmD, Sarah E. Anthony, MSc, Addison Kimber, BA, Dr. John P. Ney, MD, MPH, Dr. Kaicheng Wang, MD, MPH, Dr. X. Michelle Androulakis, MD, Dr. Melinda Thiam, MD, Dr. Brenda T. Fenton, PhD, Dr. Elizabeth K. Seng, PhD, and Dr. Jason J. Sico, MD, MHS, an algorithm could implement the definition to identify patients with RM.