Blood Markers of Neurodegeneration Higher in COVID-19 Than in Alzheimer Disease
In a study published in Alzheimer's Disease and Related Disorders, it was found that individuals hospitalized with COVID-19 had elevated blood markers of neurodegeneration similar to individuals with Alzheimer disease (AD).
Participants (n=251, average age 71) with no symptoms of cognitive decline or dementia before hospitalization with COVID-19 were characterized by whether they had neurologic symptoms and by recovery and discharged vs continued hospitalization or death. The COVID study data was compared with the data of the NYU AD Research Center (ADRC) Clinical Core cohort.
"Our findings suggest that patients hospitalized for COVID-19, and especially in those experiencing neurological symptoms during their acute infection, may have levels of brain injury markers that are as high as, or higher than, those seen in patients with AD," says lead author Jennifer A. Frontera, MD, professor in the Department of Neurology at NYU Langone Health.
Markers of toxic metabolic encephalopathy (TME)—glial fibrillary acidic protein (GFAP), neurofilament light (NfL), and ubiquitin carboxy-terminal hydrolase L1 (UCHL1) were compared between the COVID-19 group and people in the AD study. Other markers of neurodegeneration, including tau, phosphorylated tau (ptau181), amyloid beta 40, and amyloid beta 42 were compared among only those with COVID-19. Blood markers in the COVID group were measured in blood serum where the AD study participants were measured in blood plasma.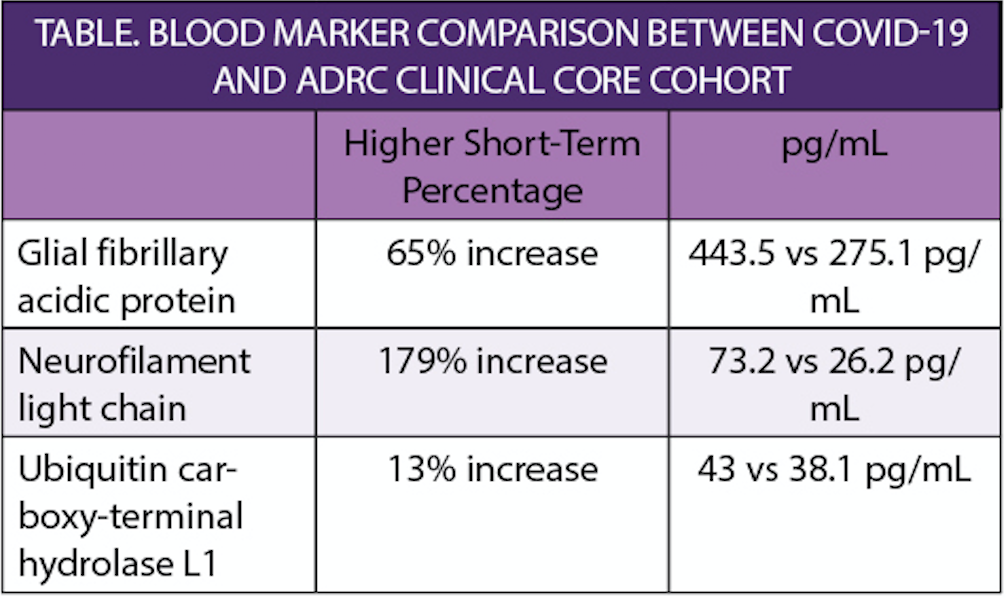
The average increase percentage in levels of the markers for participants with TME compared with participants without neurological symptoms was 60.5%.
In the COVID-19 group, the average percentage increase when comparing people who discharged home from the hospital to those who died in the hospital was 124%.
"Traumatic brain injury, which is also associated with increases in these biomarkers, does not mean that a patient will develop AD or related dementia later on, but does increase the risk of it," says senior author Thomas M. Wisniewski, MD, the Gerald J. and Dorothy R. Friedman professor in the Department of Neurology and director of the Center for Cognitive Neurology at NYU Langone. "Whether that kind of relationship exists in those who survive severe COVID-19 is a question we urgently need to answer with on-going monitoring of these patients."
