Diagnosis and Treatment of Vasculitic Neuropathy
The vasculitides are a heterogeneous group of disorders that may affect any organ or tissue in the human body. Vasculitis causes inflammation in the blood vessels that leads to ischemia and tissue damage; the clinical symptoms of the vasculitis depend on the tissues involved. Most often, vasculitis is a systemic disease, in which multiple organs are involved; however, single organ vasculitis exists. Vasculitic neuropathy (VN) arises when the peripheral nervous system is involved. VN can be isolated to the peripheral nervous system (ie, nonsystemic VN [NSVN]) or occur as part of a systemic disease (ie, systemic VN [SVN]).
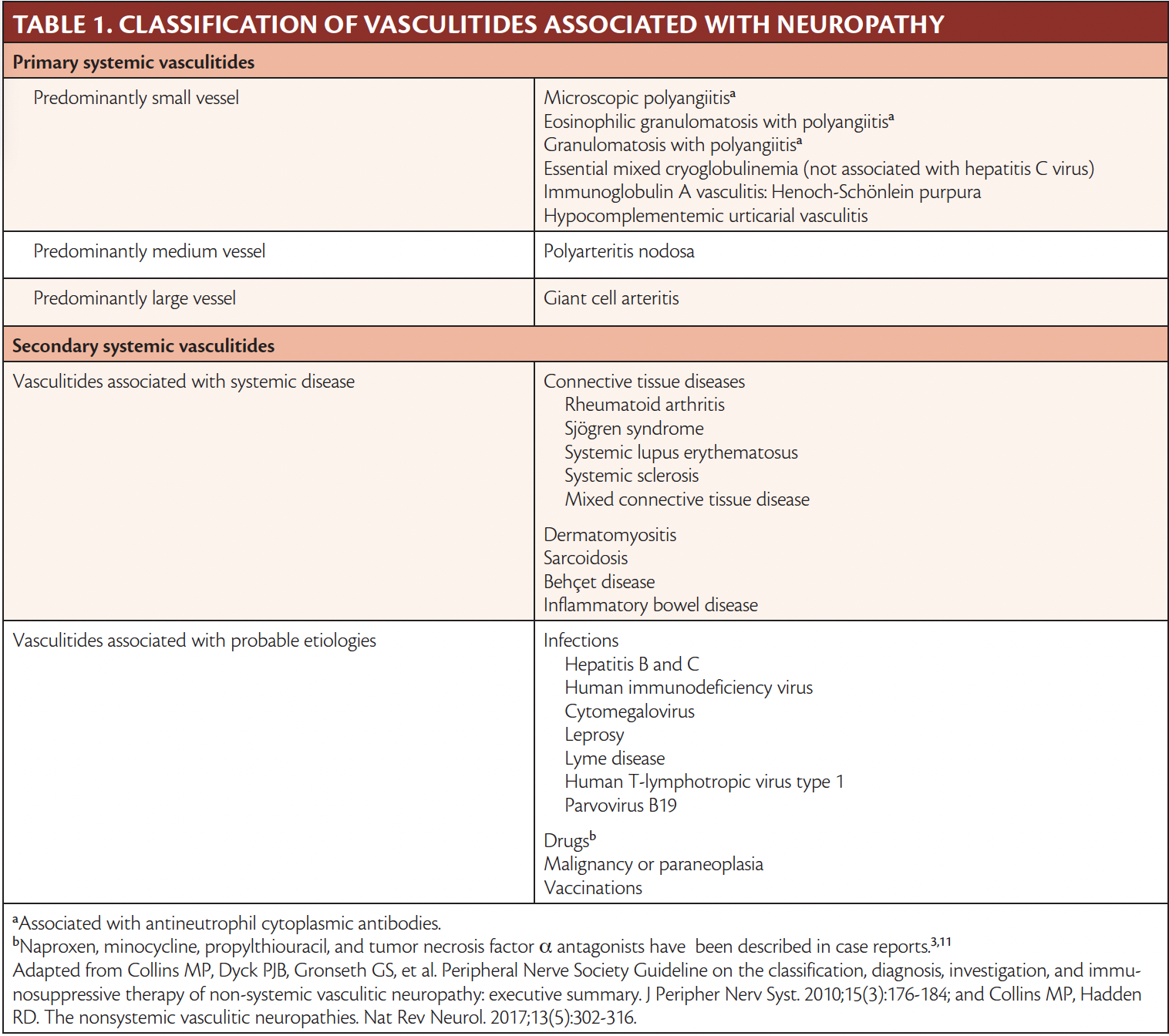
In 2010, the Peripheral Nerve Society published a guideline to the classification and diagnosis of VN, as well as recommendations for the treatment of NSVN, based on the literature.1 Table 1 shows the classification of the vasculitides associated with neuropathy. Among the primary systemic vasculitides, those that affect the small to medium-sized blood vessels are particularly associated with VN. For example, VN occurs frequently in individuals with polyarteritis nodosa (65% to 85%),2,3 eosinophilic granulomatosis with polyangiitis (60% to 80%), cryoglobulinemic vasculitis (30% to 70%), and microscopic polyangiitis (40% to 50%),2,4 whereas it is rarely seen in giant cell arteritis (5%).5 Other systemic diseases in which VN occurs are systemic lupus erythematosus (20% to 27%), rheumatoid arthritis (15% to 70%), and Sjögren disease (30% to 45%).3
In recent years, several syndromes have been proposed to be classified as NSVN, including Wartenberg migratory sensory neuropathy, nondiabetic and diabetic radiculoplexopathy, and some types of neuralgic amytrophies.6,7 Thus, NSVN includes both more benign and often self-limiting conditions as well as chronic and progressive diseases.
The overall prevalence of VN remains unknown, but nerve biopsy verified studies have implied that NSVN constitutes approximately 28% of all VN.2 Based on the heterogenic clinical phenotypes described in the following, it is generally accepted that VN, and especially NSVN, is underdiagnosed.
Clinical Features
VN is typically associated with an acute to subacute painful onset involving 2 or more individual sensory, motor, somatic, or sensorimotor peripheral nerves, resulting in asymmetric dysesthesias, paresthesias, and palsies.6,8 This presentation is referred to as mononeuritis multiplex. VN is a possible cause for mononeuritis multiplex, but there are multiple differential diagnoses, as illustrated in Table 2. Although mononeuritis multiplex is the classic phenotype, VN may present as a distal sensorimotor polyneuropathy or as a plexopathy, as illustrated in Figure 1. The distal nerves in the lower limbs are often affected first. The common peroneal (ie, fibular) nerve is affected in approximately 90% of individuals, whereas the ulnar nerve is the most commonly affected nerve in the upper limbs (58% of cases). Cranial nerves are only affected in approximately 6% of individuals.2,7 As time passes, the mononeuropathies may converge, and the symptoms imitate a distal, symmetric, or asymmetric polyneuropathy.
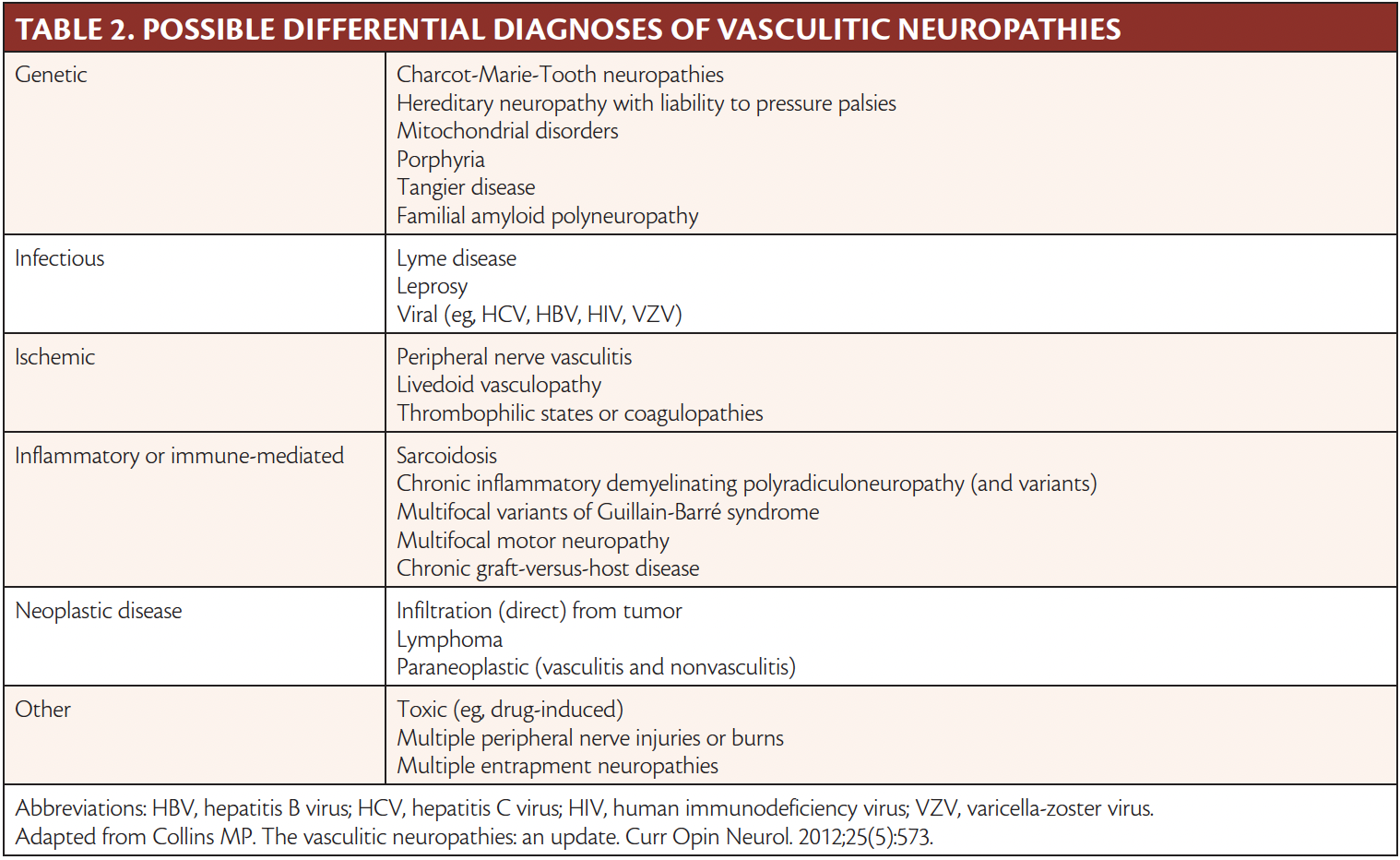

Figure 1. Patterns of nerve involvement in vasculitic neuropathy. Mononeuritis multiplex with simultaneous involvement of different peripheral nerves (A). With progression from A, sequential involvement of more nerves, leading to an early overlapping mononeuritis multiplex (B). Further progression from B, leading to an asymmetric polyneuropathy, where the distributions of several different nerves overlap (C). Distal sensorimotor polyneuropathy (D). Plexopathy (E).
Adapted from Collins MP, Hadden RD. The nonsystemic vasculitic neuropathies. Nat Rev Neurol. 2017;13(5):302-316.
NSVN predominantly involves both sensory and motor peripheral nerves, but pure sensory involvement is seen in up to 15% of cases, whereas pure motor presentation is rare.6,9 Forty-five percent of individuals will present with an asymmetric polyneuropathy, and 20% with a distal symmetric polyneuropathy. Five to ten percent of individuals with NSVN present with an acute onset and rapidly progressive course, whereas 50% have subacute, relapsing progression, and 40% have a chronically progressive course.7 Despite the common perception that NSVN is not a systemic disease, a considerable share of individuals present with constitutional symptoms (eg, 30% have clinically significant weight loss and 10% have prolonged unexplained fever).6,7,10 In comparison, constitutional symptoms, such as weight loss, fever, or fatigue, are seen in 80% of individuals with SVN.3 Moreover, 20% of individuals with NSVN have no pain.4,6,7 This heterogeneous presentation of NSVN combined with limited paraclinical findings may explain why the median time to diagnosis has been reported to range from 2.5 to 24 months, with delay reported up to 13 years.6
Investigations and Diagnosis
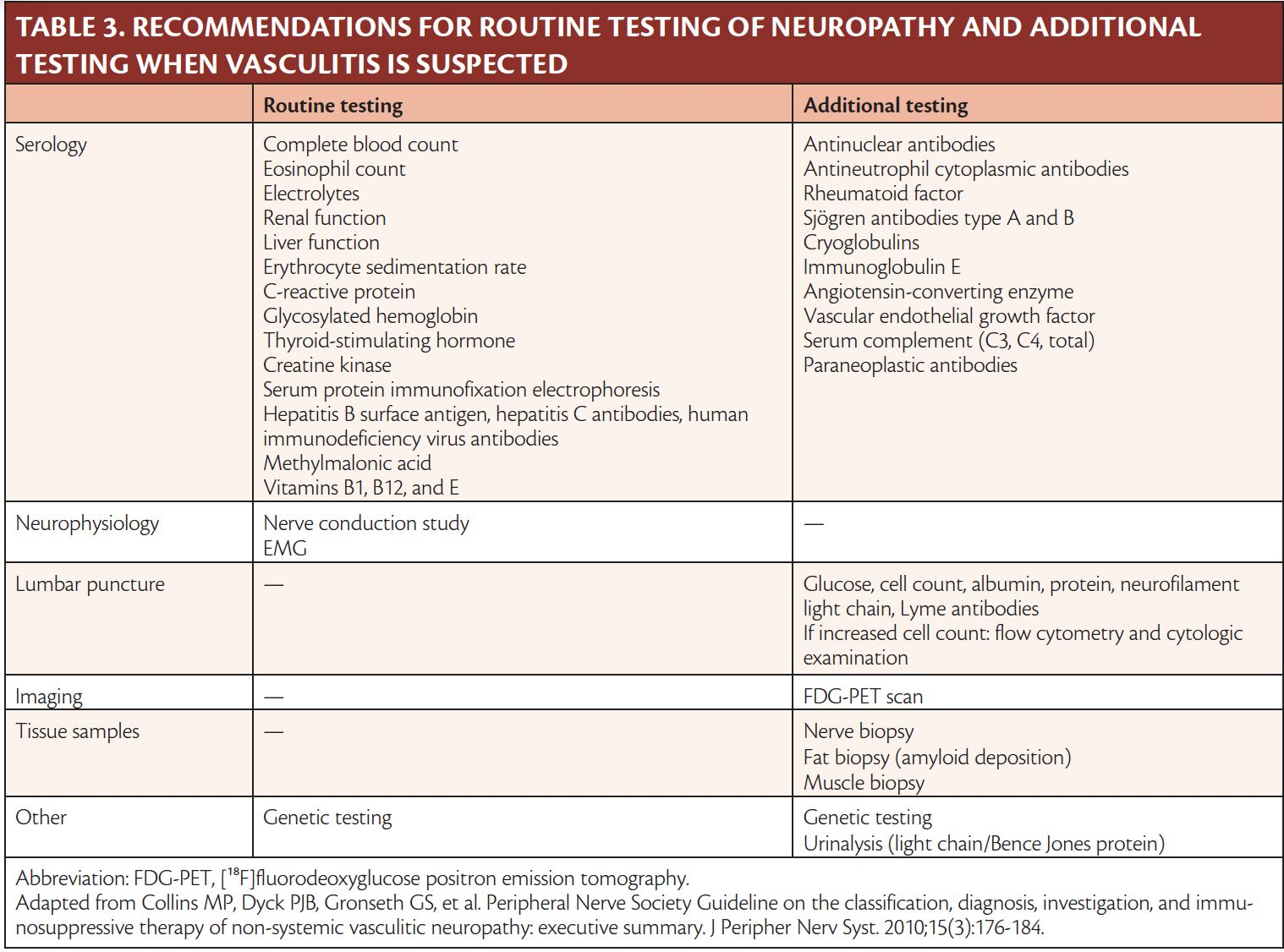
The diagnosis of peripheral neuropathy is based on a thorough medical history as well as a physical and neurologic examination followed by the relevant testing. A rapidly progressing course with objective sensorimotor impairment with or without constitutional symptoms may raise the suspicion for VN. It is essential to screen for specific organ involvement to uncover any underlying systemic disease, as several of these have a high mortality rate. Paraclinical investigations are therefore often extensive, as illustrated in Table 3.
Nerve conduction studies will reveal a sensorimotor or pure sensory axonal neuropathy in several individual peripheral nerves, often in an asymmetric or multifocal pattern. EMG will show diffuse denervation in affected nerves or muscles.4,6,11 Electrodiagnostic studies may also reveal a subclinical asymmetry, and identify a relevant site for nerve biopsy (see the following).
The diagnosis of VN is based on pathologic evidence of vasculitis in a nerve biopsy, as described in the 2010 Peripheral Nerve Society guidelines1,6 and illustrated in Figure 2. A nerve biopsy can be omitted if vasculitic changes have been detected in another organ. It is important to choose a clinically, electrodiagnostically, or radiographically affected nerve, and often an easily accessible sensory nerve (eg, sural, superficial peroneal [fibular], superficial radial) will be chosen. Pathologic features include multifocal nerve fiber loss with varying degrees of axonal degeneration, hemosiderin-laden macrophages, immune complex deposition, neovascularization, perivascular inflammation, and fibrinogen in epineurial vessel walls.8 The diagnostic sensitivity of a nerve biopsy is challenged by factors including the segmental effect on the nerves, such that the primary site of involvement may be proximal to the nerve biopsy. The nerve may also be degenerated, thus lacking diagnostic disease activity at the biopsy site. The risk of overlooking vasculitic changes is reduced by examining the nerve on serial sections.12 Concomitant muscle biopsy has been shown to increase sensitivity by 5% to 25% in VN.8,13 If a nerve biopsy cannot be performed in a relevant nerve, or if the histopathologic findings are inconclusive, it is possible to make the diagnosis of clinically probable VN.1 The diagnosis of NSVN relies on the previously mentioned data and exclusion of any systemic disease that may cause VN.1
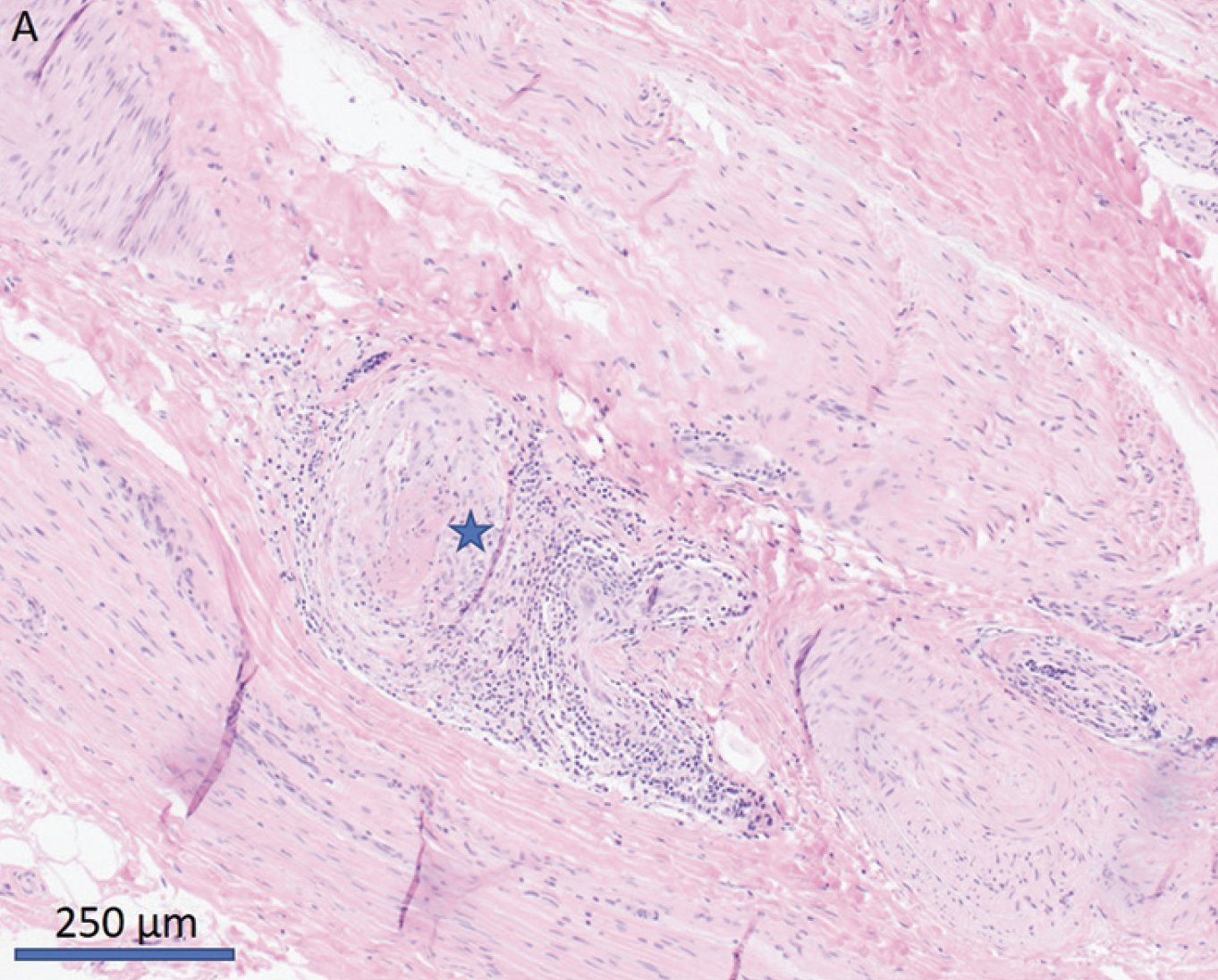
Figure 2. Sural nerve biopsy with vasculitic changes in a perineural blood vessel. Infiltration of inflammatory cells in the vessel wall and thrombosis is noted. The vasculitic changes were segmental and were not present in different sections of the biopsy.
Reprinted with permission from Witt AM, Kodal LS, Pedersen BS, Lund EL, Dysgaard T. Fejltolkning af nonsystemisk vaskulitneuropati medfører forsinket behandling. Ugeskr Laeger. 2023;185(18):V10220665.
Treatment
Treatment of VN depends on the underlying etiology. The aim is to stop ongoing nerve damage and prevent further disease progression. In SVN, treatment will be based on the underlying systemic disease, and will typically take place in the relevant medical specialty. If an immunologic cause is suspected without signs of another underlying disease, the treatment is immunosuppressive medication. Whether the vasculitic activity in peripheral nerves and other organs has the same course, or if immunosuppressive agents are equally effective in treating the neuropathy, is unknown. Therefore, disease activity must be monitored in involved organs, including the peripheral nerves, during treatment.
No prospective data on NSVN treatment have been reported. The current recommendations (from 2010) are based on clinical experience, observational studies, and extrapolation of data from studies on treatment of systemic vasculitis.1 Treatment of NSVN traditionally has been less aggressive than treatment of SVN, which left untreated is associated with a high mortality rate. Assessment of disease activity and thus indication for initiating treatment of NSVN relies on the physician, but there are no guidelines for grading the activity of NSVN. According to the 2010 Peripheral Nerve Society recommendations, first-choice treatment is glucocorticoid monotherapy. In the case of an aggressively ongoing NSVN or disease progression on glucocorticoids, 18 to 24 months of combination therapy with a glucocorticoid and a glucocorticoid-sparing agent (eg, cyclophosphamide, methotrexate, azathioprine) is recommended.1 Most recently, rituximab has been mentioned as a possible treatment of VN based on studies of systemic vasculitis.6,8,14,15
There is a growing consensus that the treatment of NSVN ought to be more aggressive, as several retrospective studies have shown that combination therapy rather than monotherapy with glucocorticoids reduces irreversible and debilitating nerve damage.6,16-18
It is recommended that individuals with VN, in addition to medical treatment, receive physical rehabilitation with regular physical training as early as possible. Aids such as ankle foot orthotics may be needed.
Prognosis
The reported data for the prognosis of VN are influenced by variation in the chosen treatment regimen. Overall, the prognosis for improvement in sensorimotor symptoms is favorable, although the outcome depends on the speed of nerve regeneration.19 Younger age is associated with a better outcome.9 The prognosis is further improved with combination therapy compared with monotherapy; relapse is seen more often in individuals with NSVN withdrawn from glucocorticoid monotherapy despite treatment response, whereas individuals on combination therapy with cyclophosphamide have fewer relapses.19 Up to 82% of individuals with NSVN on immunosuppressive treatment will regain or maintain the ability to walk without aids, and only 3% will have ceased walking function.6
Pain is a dominant problem in many individuals with VN, and 44% to 71% of individuals with an otherwise good response to treatment will have chronic pain, which can prove difficult to treat.4,16,19 To date, no studies have measured the effect of treatment on neurologic outcomes in individuals with SVN.
Conclusion
VN is commonly seen in individuals with primary or secondary systemic vasculitis, but also as a single-organ vasculitis. The clinical presentation is heterogeneous, and ranges from acute, painful, asymmetric, sensorimotor neuropathy to a slowly progressive, symmetric, sensory polyneuropathy. NSVN, in particular, can differ from mononeuritis multiplex, which is considered the classic phenotype. This makes diagnosis difficult and results in diagnostic delay and underdiagnosis. Therefore, it is important to suspect VN in unexplained persistent, progressive sensory or sensorimotor axonal neuropathy, particularly when pain is present.
When VN is suspected, thorough investigations are of utmost importance, because VN may be associated with systemic diseases with high morbidity and mortality rates if untreated.
Treatment of VN is by means of immunosuppression; however, no prospective studies on VN treatment have been performed. A more aggressive approach to the treatment of NSVN shows better outcome on remission compared with monotherapy with glucocorticoids.
Investigations are needed into the natural history, treatment, and pathogenic mechanisms of VN to increase our understanding of this disease.
Ready to Claim Your Credits?
You have attempts to pass this post-test. Take your time and review carefully before submitting.
Good luck!
Recommended
- Neuromuscular
The Consequences of Delays in the Diagnosis of Generalized Myasthenia Gravis
John A. Morren, MD, FAAN, FAANEMJohn A. Morren, MD, FAAN, FAANEM - Neuromuscular
A Case of Adult-Onset Postviral Opsoclonus–Myoclonus Syndrome
Vivian Chen, MD; Anivarya Kumar, MDVivian Chen, MD; Anivarya Kumar, MD



