An Alternative Pathway to the ABPN Maintenance of Certification
Maintenance of Certification (MOC) has recently become a cause célèbre throughout the entire practice of medicine. Of course, MOC is just one of several burdens of dubious value in the name of “quality” with which physicians are saddled. Physicians must also meet the demands of interested parties, including Medicare, private insurance companies, and various consumer and patient advocacy groups. Meanwhile, we must also satisfy measures for Physician Quality Reporting System (PQRS) and ICD-10. MOC, if not the most onerous of the demands, is at least the most immediate one, and it also offers arguably the best opportunity for alternative means of compliance.
MOC in neurology: Origins and current framework
The American Board of Psychiatry and Neurology, Inc. (ABPN) was founded in 1934, and is one of the 24 member boards of the American Board of Medical Specialties (ABMS). The mission of the ABPN is to serve the public interest and promote excellence in the practices of psychiatry and neurology. With approval from the ABMS, the ABPN also instituted board certification in neurology sub-specialties in clinical neurophysiology, pain medicine, neurodevelopmental disabilities, vascular neurology, neuromuscular medicine, sleep medicine, epilepsy, brain injury medicine, as well as hospice and palliative medicine.1
Physicians who completed board certification prior to October 1, 1994 were granted lifetime certificates. For diplomates seeking initial board certification after this date, time-limited certificates were issued, and the ABMS mandated re-certification for these diplomates. As such, after 10 years, neurologists were required to take a re-certification examination in addition to meeting the usual CME requirements to maintain an active medical license. In 2007, the ABMS mandated that the recertification programs of its subsidiary boards would transition to what today is referred to as Maintenance of Certification programs.1 In addition to the 50-100 hours of CME required every two years (by most states) and a recertification written examination every 10 years at a cost of over $1,500 to physicians, the ABPN also agreed to additional ABMS requirements for MOC, including the so-called Self Assessment (SA) modules and Improvement in Medical Practice (PIP) modules.
According to the ABPN website, “the change from recertification to MOC strengthened the program and guaranteed that physicians were current in ways not immediately available for testing.” At the same time, the ABPN/ABMS determined that these standards should not apply to Diplomates who had completed board certification prior to October 1, 1994, thereby holding “grandfathered physicians” to a lower standard than the rest of their peers, notwithstanding that many of the older physicians—who are many years out of their residency training—may be among the ones who are least up to date with current practice.
high cost, low value
MOC is at best a dubious concept with unclear goals. What the public and physicians alike want to ensure is that all professionals charged with maintaining and protecting the health of patients are competent in what they do. The initial board certification process traditionally has been an attempt to do just that—to show that a board candidate can demonstrate a basic competency as a physician in his or her chosen field. On the other hand, the current ABMS/ABPN MOC requirements do not and cannot assure that a practicing physician has maintained his or her competency to practice neurology or a neurologic subspecialty, or even to practice medicine, for that matter. The ABMS acknowledges this concept. In fact, one ABMS member website has included the following statement: “Many qualities are necessary to be a competent physician, and many of these qualities cannot be quantified or measured. Thus, certification is not a guarantee of the competence of the physician specialist.” In other words, board certification is meant to demonstrate competence, but the board does not want to guarantee competence.2 This concept also nullifies the notion that the American College of Physicians (ACP) raised, that if you become involved in litigation, Board certification will somehow protect you.3 The fact is that if you are negligent, no piece of paper hanging on your wall will protect you.
The ABMS requirements for MOC (see sidebar) are arbitrary and untested. The costs to practicing neurologists both in terms of time and money to complete this process are considerable. In a recent study, physician compliance with MOC was found to cost anywhere from $23,607 to $40,495 over a 10-year period depending on specialty.4 Yet, there is no published evidence to show that any of these requirements except for Continuing Medical Education (CME) serve to improve quality of practice on an individual basis. No one would argue that CME is irrelevant, and most states require CME (25-50 hours of accredited CME per year) for maintenance of licensure.
MOC REQUIREMENTS
• Professionalism and Professional Standing
• Lifelong Learning (CME) and Self-Assessment (Beginning January 1, 2014, diplomates are required to use only ABPN-approved products for self-assessment activities, which are found on the ABPN website (www.abpn. com). The ABPN will approve additional programs over time and reserves the right to approve or reject any course or guideline submitted for approval.)
• Assessment of Knowledge, Judgment, and Skills
• Improvement in Medical Practice (PIP), which consists of a Clinical Module (initial chart review and 2 year reassessment of at least five patients, assessing the charts for adherence to best practices, practice guidelines, peer standards, and then developing and carrying out a plan to improve clinical effectiveness and/or efficiency), and a Feedback Module (from which the Diplomate can choose ONE, including peer feedback from five peers, resident evaluation from five respondents, 360 degree evaluation from five respondents, institutional peer review from five respondents, and supervisor evaluation from one supervisor
Criticism, Controversy, and Public Perception
Over the last year, much criticism has been directed against MOC and there is some evidence that the issue begun to take hold publicly. For example, in a recent overview of the MOC issue published in The New England Journal of Medicine (January 8, 2016), Dr. Paul Teirstein, Chief of Cardiology at the Scripps Clinic, criticized the financial aspects of MOC as they apply to both individual physicians and the ABMS and its subsidiary Boards, in this case the American Board of Internal Medicine (ABIM).5 Shortly after this article appeared, the ABIM issued a “mea culpa” and suspended some of the Practice Assessment, Patient Voice and Patient Safety requirements for at least two years.6
MOC has breached the lay media, as well. Newsweek’s Kurt Eichenwald has written multiple pieces on MOC, covering problems with board certification, as well the exuberant salaries, bonuses, and luxurious perks that the ABMS has been awarding itself at the expense of its Diplomates.7,8 And yet, in response to these reports, the ABIM accused Mr. Eichenwald of being biased because he is married to a physician.9
While the public perceives correctly that there are major problems with medicine and our health care delivery system, often misidentified are both the causes and the solutions. Ironically, the proposed solution to add more unnecessary administrative and regulatory requirements to an already labyrinthine system actually compounds rather than mitigates the problems.
We all know that most medical errors and complications have little to do with individual providers being out of date, per se, other than in the case of impairment due to age and illness, which is a separate problem entirely and must be addressed directly. Much is the result of the lack of a systematic and rigorous approach to the provision of care along the lines of what Atul Gawande and others have been writing about for years. When physicians are encouraged—even forced—by the system to spend no more than 15-20 minutes with a patient, much of which already consists of checking off senseless bullet points on an EHR screen, all the up-to-date knowledge in the world is not going to help them provide better care. Patient advocacy groups and politicians do not appear to understand this concept, however.
The other unfortunate irony is that re-licensure and recertification burdens will not likely weed out the bad actors, but may rather serve to annoy and frustrate the good ones. The challenge is to educate the public and the patient advocacy groups as to what should be done to reduce the inadequacies they perceive in the system (some of which are very real), rather than to accede to their own poorly conceived remedies for problems they do not really understand. To charge them with making medical policy is like having a physician instruct a mechanic on how to repair car brakes. Such instruction may be well intentioned enough, but would likely result in the car being unsafe to drive.
Action and Reaction
On February 24, 2015, former American Academy of Neurology (AAN) President Timothy A. Pedley, MD, FAAN, issued a statement on behalf of the AAN arguing that Part IV of MOC is an onerous requirement, and that this ABPN requirement has imposed a hardship on neurologists. The statement also reinforces the idea that the process is unnecessarily cumbersome, especially in the absence of convincing research demonstrating that it is effective in improving physicians’ practice and the quality of the care they provide.
On March 2, 2015, the American Board of Medical Specialties (ABMS) issued a disappointing response letter that failed to acknowledge even the changes that the ABIM had already conceded for its own diplomates; changes that the vast majority of ABPN diplomates would like to see enacted.
In July 2015, the ABPN announced that as of January 1, 2016, “the Feedback Module (patient or peer surveys) will become a highly recommended yet optional component for all ABPN diplomates enrolled in Maintenance of Certification. The Part IV Clinical Module component (chart review) will remain a requirement.” This decision was attributable to pressure from physicians and physician groups like the AAN. It was a step in the right direction, to be sure, but a far cry from adequate reform.
A New Pathway
Fortunately, there is a viable alternative to the ABMS/ABPN pathway to MOC. The National Board of Physicians and Surgeons (NBPAS), which was started by Dr. Paul Teirstein, is offering recertification in selected medical specialties. The Board of Directors of the NBPAS comprises members representing many of the country’s top clinics, academic institutions, and specialty organizations (See Figure 1). All physician members and directors of the NBPAS are volunteers (there is a small paid administrative staff, of course), in contradistinction to the ABMS and its member Boards, in which the members of these Boards are paid in six figure dollar amounts annually. (For a sample tax form, visit the following link: http://990s.foundationcenter.org/990_pdf_archive/410/410654864/410654864_201212_990O.pdf)
The NBPAS has established the following criteria (NBPAS.org) for its recertification:
• Previous certification by an ABMS member Board
• Valid license to practice medicine
• At least 50 hours of ACCME accredited CME within the past 24 months (physicians-in-training are exempt)
• Active hospital privileges (for select specialties)
• Clinical privileges in certified specialty have not been permanently revoked
• Cost: $169 for a two-year certification, not including the cost of obtaining CME credits
The MOC requirement itself is incorporated in Medicare law and under the Patient Protection and Affordable Care Act (PPACA), although there is ambiguity regarding whether MOC must be obtained via the ABMS Specialty Boards. When these laws were written, the ABMS was essentially “the only game in town” for physicians. The ABMS has been challenged in terms of being a monopoly organization for specialty certification and recertification. Presumably because of this, or perhaps as a pre-emptive defense, the ABMS has recently acknowledged publicly that it does have competition in the form of the NBPAS. To punctuate this point, one ABMS member website has included the following statement, “Possession of a Board certificate does not indicate total qualification for practice privileges, nor does it imply exclusion of other physicians not so certified.”2
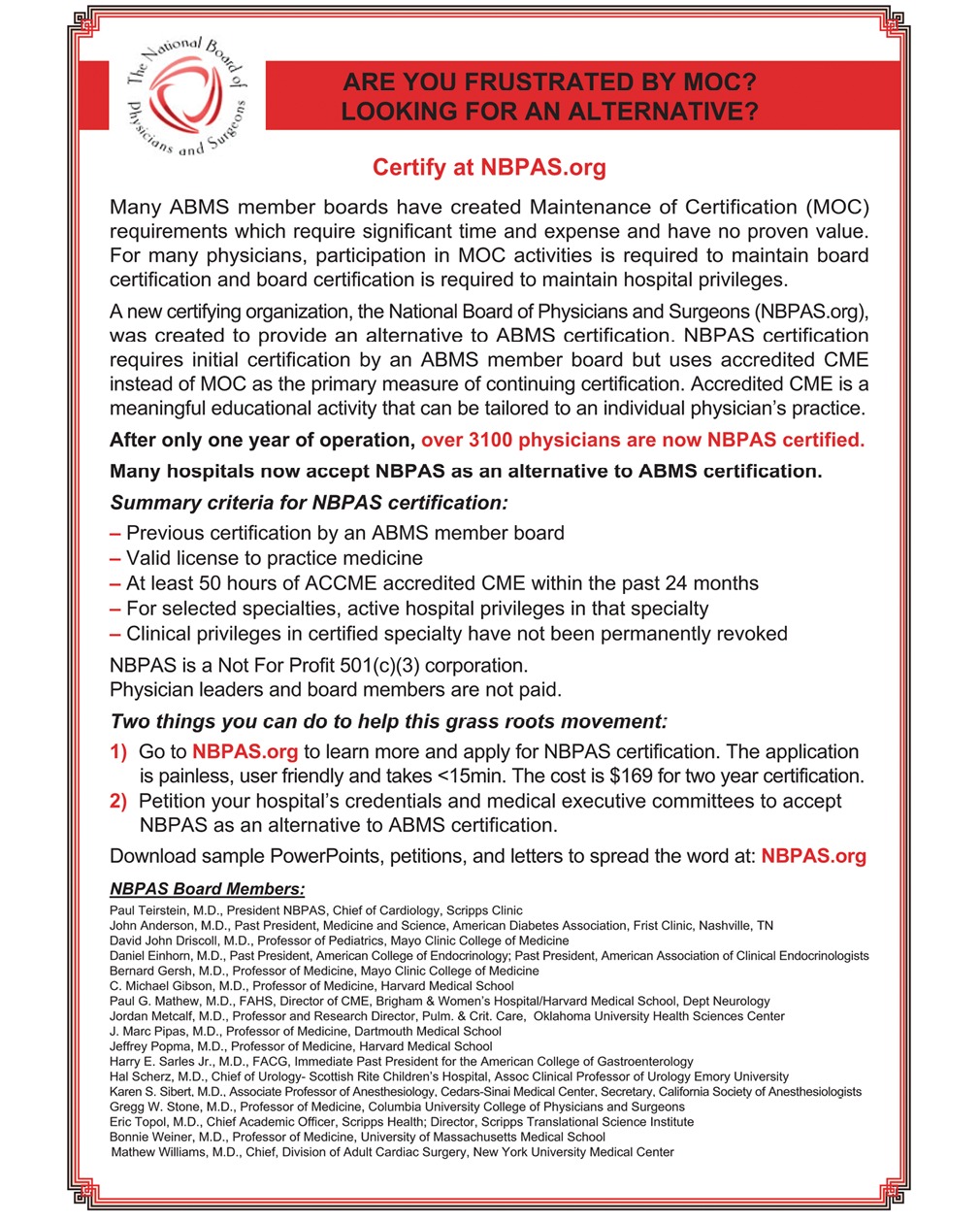
Figure 1. An ad by the National Board of Physicians and Surgeons (NBPAS.org) appearing in The New England Journal of Medicine.
Due to pressure NBPAS and others the ABMS boards have had to reconsider their position on MOC. Beginning in 2016, the American Board of Anesthesiology decided to discontinue their 10-year recertification examination. Instead, their diplomates will be taking an online 30-question quiz per calendar quarter (120 questions per year). Many of the previous requirements remain in place. Although this is a step in the right direction, one must assume that making a 120 question, online, open-book exam for all diplomates recertifying is significantly cheaper to produce and administer than a secured 10-year exam. That being said, the cost of this new MOC program is $210 per year instead of a lump sum $2,100 to take the closed book exam every 10 years.10,11 Clearly, the boards feel a reduction in cost of production to the boards should not translate to a reduction in cost to the diplomates, and that the boards should actually generate even greater revenues.
The ABPN has also responded positively by forming an MOC clinical advisory committee to work provide suggestions and feedback on how MOC impacts practice and “potentially” improves patient care.11 Their use of the word “potentially” when referring to MOC improving care is particularly encouraging, because it implicitly suggests that evidence needs to be found to support that claim.
The Future of Board Certification
Despite the mild progress we have seen, I have voiced my concerns to ABPN and AAN leadership.
Meaningful MOC reform should include all of the following:
• Removing the 10-year recertification exam.
• Lowering the cost of MOC if a quarterly online question format is put in place. Keeping the same fee structure would be ridiculous considering the expense to the ABPN is much smaller for this than generating and administering a 10-year exam. Participants should receive CME credit for completing these online modules.
• Removing unnecessary, cumbersome, and unproven modules (PIP & SAE).
• Basing re-certification primarily on CME and a clean practice record.
The ABMS boards acknowledge that the National Board of Physicians and Surgeons (NBPAS) exists as a legitimate alternative board, but they do not feel threatened at all.13 They are very confident that physicians, like sheep to be herded, will continue to blindly pay to do unnecessary work in the name of board certification.
Unfortunately for the ABMS boards, more physicians are starting to understand that there is now another pathway to re-certification. Over 3,000 physicians have become diplomates of NBPAS, which has become accepted as a viable alternative to ABMS by an increasing number of hospital credentialing departments. It is only through an expanding number of diplomates that NBAPS can increase its acceptance and rival the inflexible, self-centered monopoly that ABMS has become. In order to attract more diplomates, a full-page advertisement (Figure 1) will be featured in The New England Journal of Medicine in four editions.
Over time, the NBPAS should grow in terms of certificates granted. Moreover, the number of hospital credentialing committees that accept NBPAS as a viable alternative for maintenance of board certification will likely increase, as well. With more institutions accepting NBPAS certification, the influence and leverage of the NBPAS will grow, and physicians will be relieved of the burden of complying with costly and time-consuming requirements that do not improve practice. It might even force the ABMS to revise its own requirements for MOC. Ultimately, it is up to the individual physician to decide whether it is to his or her advantage to take a stand on MOC, based upon principle. There is no harm in being dual-boarded, and becoming a diplomate of NBPAS prior to the expiration of an ABPN/ABMS board certification is a low risk decision that supports a pro-physician grassroots movement. During this time of unprecedented physician unity, organizations like NBPAS appear well positioned to help return the practice of medicine to physicians rather than detached administrators. n

Paul G. Mathew, MD, FAHS is Co-Chief Medical Editor of Practical Neurology® and a member of the Harvard Medical School faculty. He is Director of Continuing Medical Education at the Brigham & Women’s Hospital and is a staff neurologist at Harvard Vanguard Medical Associates and the Cambridge Health Alliance. He also serves as the neurology representative on the volunteer advisory board of the National Board of Physicians and Surgeons.
1. http://www.abpn.com/about/mission-and-history/
2. https://www.abpmr.org/consumers/consumers.html
3. http://www.acponline.org/education_recertification/recertification/moc_email_to_members_2.20.15.pdf
4. Sandhu AT, Dudley RA, Kazi DS. A Cost Analysis of the American Board of Internal Medicine’s Maintenance-of-Certification Program. Ann Intern Med. 2015 Jul 28. doi: 10.7326/M15-1011. [Epub ahead of print]
5. Teirstein, PS. Board to the Death—Why Maintenance of Certification is Bad for Doctors and Patients. N Engl J Med 2015; 372:106-108. http://www.nejm.org/doi/ref/10.1056/NEJMp1407422#t=article
6. http://www.abim.org/news/abim-announces-immediate-changes-to-moc-program.aspx.
7. http://www.newsweek.com/2015/03/27/ugly-civil-war-american-medicine-312662.html
8. http://www.newsweek.com/medical-mystery-making-sense-abims-financial-report-334772?rel=most_read3
9. http://www.medscape.com/viewarticle/842040
10. http://www.theaba.org/MOCA/About-MOCA
11. http://www.theaba.org/PDFs/MOCA/MOCA-2-0-FAQs
Ready to Claim Your Credits?
You have attempts to pass this post-test. Take your time and review carefully before submitting.
Good luck!
Recommended
- Practice Management
Microplastics and "Negative Neuroplasticity": An Emerging Topic in Clinical Neurology
Keshav Shah, MBBS; David Davis, PhDKeshav Shah, MBBS; David Davis, PhD - Practice Management
The Myth of Medical Gaslighting: When Patient Perception and Physician Intention Collide
Joseph A. Hirsch, PhD; Manijeh Berenji, MD, MPHJoseph A. Hirsch, PhD; Manijeh Berenji, MD, MPH - Practice Management
Physicians with Substance Use Disorder, Part I: Overview and A Personal Journey Through Recovery
Chris Bundy, MDChris Bundy, MD



